Brachytherapy is the placement of radioactive sources in or just next to a tumor. During brachytherapy, the radioactive sources may be left in place permanently or only temporarily, depending upon your cancer.
There are two main forms of brachytherapy – intracavitary treatment and interstitial treatment. With intracavitary treatment, the radioactive sources are put into a space near where the tumor is located, such as the cervix, the vagina or the windpipe. With interstitial treatment, the radioactive sources are put directly into the tissues, such as the prostate. Another use of brachytherapy is surface mold brachytherapy, which can be used externally to treat some skin cancers.
Depending on the technique, radiation therapy dose from brachytherapy can be delivered with one of two different dose rates – high-dose-rate (HDR) or low-dose-rate (LDR). With HDR brachytherapy, radiation dose is deposited at a faster rate. LDR brachytherapy emits radiation at a slower rate.
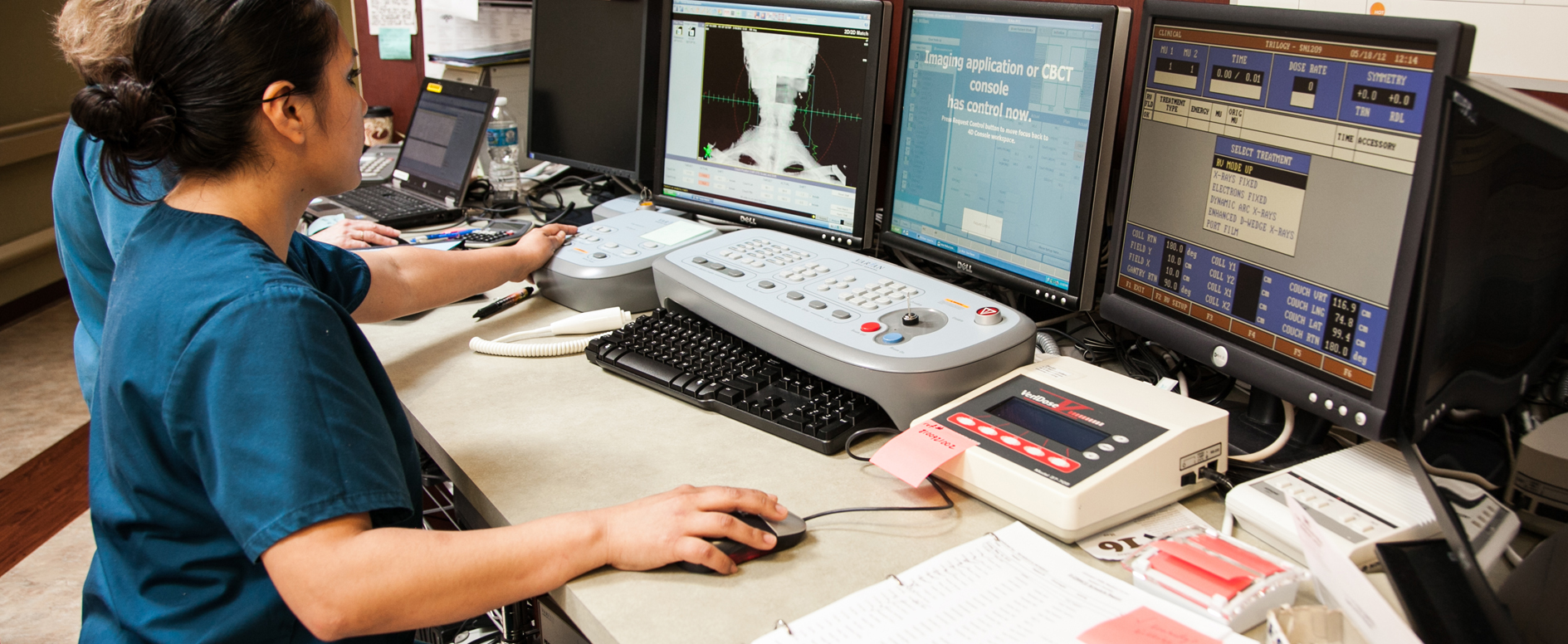
HDR brachytherapy involves the temporary placement of a powerful radiation source, accurately directed by your radiation oncologist and team. It is delivered into the tumor through a tube called a catheter. It is usually given in multiple doses once or twice daily or once or twice weekly. This procedure may require anesthesia and a surgical procedure. Your doctor and team will control this treatment from outside the treatment room, monitoring you as the therapy is being given. Devices called high-dose-rate remote afterloading machines allow the team to deliver treatments quickly. You may be able to go home shortly after the procedure, resuming your normal activities with few restrictions.
LDR brachytherapy involves the placement of temporary or permanent radiation sources into the tumor area. Placement of permanent radiation sources often require anesthesia, a surgical procedure and a brief stay in the hospital. Patients with permanent implants may have a few restrictions at first and then can quickly return to their normal activities. Temporary implants are left inside the body for minutes, hours or days, depending on the type of brachytherapy. While the temporary radioactive sources are in place, patients stay in a private room. During this period, doctors, nurses and other medical staff will continue to take care of patients, but they will take special precautions to limit their exposure to radiation. Once the temporary implants are removed, these patients have few restrictions and can quickly return to their regular routine.
Most patients feel little discomfort during brachytherapy. If the radioactive source is held in place with an applicator, you may feel discomfort from the applicator. There are medications that can relieve this discomfort. If you feel weak or queasy from the anesthesia, ask your team for medication to help you feel better.
Depending on the type of brachytherapy you receive, you may need to take some precautions after you leave your treatment, particularly if you plan to be around young children or pregnant women. Because temporary implants are removed after treatment, these radiation safety precautions apply mainly with permanent implants. Ask your radiation oncologist or radiation oncology nurse about anything special you should know. Brachytherapy may be used alone or in combination with external radiation treatments. Your radiation oncologist will advise you if these treatments are appropriate for you.